postpartum depression screening scale pdss pdf
The Postpartum Depression Screening Scale (PDSS) is a 35-item self-report tool developed by Beck and Gable in 2000 to assess postpartum depression in mothers․
It evaluates seven key dimensions of depressive symptoms‚ providing a structured format for early detection and referral of at-risk women‚ with administration lasting just 5-10 minutes․
The PDSS is specifically designed for postpartum use‚ offering a detailed yet efficient screening solution that is widely used in clinical settings and available for purchase․
Overview of Postpartum Depression (PPD)
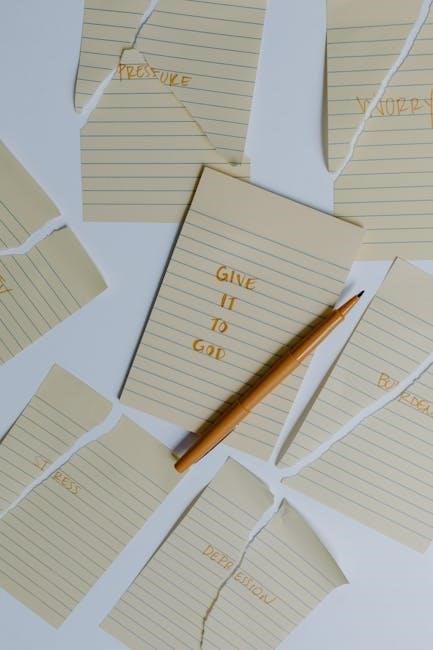
Postpartum depression (PPD) is a common mental health condition affecting women after childbirth‚ typically within the first year postpartum․
Characterized by persistent sadness‚ emotional detachment‚ and loss of interest in activities‚ PPD can interfere with a mother’s ability to care for herself and her child․
Hormonal changes‚ sleep deprivation‚ and psychological stress are key contributors to its development․
PPD can vary in severity‚ from mild symptoms to debilitating episodes requiring medical intervention․
Left untreated‚ it may impact maternal-infant bonding‚ family relationships‚ and overall maternal health․
Early identification through tools like the PDSS is critical for timely intervention and improved outcomes․
PPD is not a sign of weakness but a treatable condition requiring compassionate care and support․
Importance of Early Screening for PPD
Early screening for postpartum depression (PPD) is crucial for identifying at-risk mothers and ensuring timely intervention․
Untreated PPD can lead to severe mental and physical health consequences for both mother and child․
Screening tools like the PDSS enable healthcare providers to detect symptoms early‚ improving treatment outcomes;
Early detection also fosters better maternal-infant bonding and reduces the risk of long-term emotional and developmental issues in children․
Moreover‚ early intervention can prevent the progression of PPD into more severe forms‚ enhancing overall maternal well-being․
Regular screening during postpartum care ensures that mothers receive the support they need‚ promoting healthier families and communities․
Thus‚ early screening is a vital step in addressing PPD effectively and improving maternal mental health outcomes․
Development and Structure of the PDSS
The PDSS‚ developed by Beck and Gable in 2000‚ is a 35-item tool assessing postpartum depression across seven domains‚ designed for clinical use and available in PDF format․
History and Creation of the PDSS
The Postpartum Depression Screening Scale (PDSS) was developed by Beck and Gable in 2000‚ building on Beck’s earlier qualitative research on postpartum depression․ Initially‚ the scale included 56 items across seven dimensions‚ but it was refined to a 35-item format for clinical practicality․ The PDSS was designed to address the need for a tool specifically tailored to postpartum women‚ distinguishing it from general depression scales․ Its creation aimed to provide clinicians with a reliable‚ self-report instrument to identify women at risk for postpartum depression early and efficiently․ The scale is available in PDF format and has been validated in various studies‚ demonstrating its effectiveness in diverse populations․ It remains a widely used tool in clinical settings for assessing postpartum depression․
Structure and Format of the PDSS
The Postpartum Depression Screening Scale (PDSS) is a 35-item self-report questionnaire designed to assess postpartum depression symptoms․ It is divided into seven key domains: emotional lability‚ mental functioning‚ sleep/eating disturbances‚ anxiety/insecurity‚ guilt/shame‚ contamination/obsessions‚ and suicidal thoughts․ Each domain contains five items‚ rated on a Likert scale‚ making the tool comprehensive yet concise․ The format is user-friendly‚ allowing women to complete it independently in 5–10 minutes․ The PDSS is available in PDF format‚ facilitating easy distribution and administration in clinical settings․ Its structured design ensures consistency in screening‚ while the self-report nature empowers women to openly share their experiences‚ aiding early detection and intervention․
Key Features of the PDSS
The Postpartum Depression Screening Scale (PDSS) offers several distinct features that make it an effective tool for assessing postpartum depression․ Its 35-item structure is divided into seven domains‚ ensuring a comprehensive evaluation of both emotional and psychological symptoms․ The Likert-scale format allows for nuanced responses‚ enhancing the tool’s sensitivity․ Designed at a third-grade reading level‚ the PDSS is accessible to a wide audience‚ reducing barriers to use․ It can be completed in just 5–10 minutes‚ making it practical for clinical settings․ Additionally‚ the PDSS includes specific cutoff scores (e․g․‚ 60 for minor depression and 80 for major depression) to guide diagnosis and intervention‚ ensuring timely and targeted support for mothers at risk․

Administration and Scoring of the PDSS
The PDSS is a 35-item self-report questionnaire administered in 5–10 minutes․ It uses a Likert-scale format‚ with scores ranging from 35 to 175․ A cutoff score of 80 indicates a positive screen for postpartum depression‚ guiding further evaluation and intervention․
How to Administer the PDSS
The PDSS is a self-administered‚ 35-item questionnaire designed for postpartum women․ It is written at a third-grade reading level to ensure accessibility․ Healthcare providers should distribute the scale in a private‚ comfortable setting‚ allowing women to complete it independently․ The tool can be administered during routine postpartum visits‚ typically within 5–10 minutes․ Providers should ensure women understand the purpose of the screening and offer assistance if needed․ The PDSS can also be integrated into electronic health records for efficient documentation․ Training for healthcare staff on interpreting results is recommended to ensure accurate identification of at-risk individuals․ The scale is available in PDF format‚ making it easy to print or distribute digitally for clinical use․
Scoring and Interpretation of Results
The PDSS is scored by summing responses across its 35 items‚ with total scores ranging from 35 to 140․ A cutoff score of 80 indicates a high risk for postpartum depression‚ while scores between 60 and 79 suggest minor or major depressive symptoms․ Scores below 60 are considered within the normal range․ The scale demonstrates strong sensitivity (91-94%) and specificity (72-98%) in identifying depressive symptoms․ Interpretation should be conducted by trained healthcare providers to ensure accurate assessment․ The results guide clinical decisions‚ such as referrals for further evaluation or treatment․ This structured approach ensures early identification and intervention‚ enhancing maternal mental health outcomes effectively․

Validation and Reliability of the PDSS
The PDSS has undergone rigorous psychometric testing‚ demonstrating strong internal consistency and reliability across diverse populations․ Validation studies confirm its effectiveness in identifying postpartum depression accurately․
Psychometric Properties of the PDSS
The PDSS exhibits strong psychometric properties‚ with high internal consistency (Cronbach’s alpha > 0․90) and robust validity․ It effectively measures seven dimensions of postpartum depression‚ including emotional distress and interpersonal relationships․ The scale demonstrates excellent sensitivity (91-94%) and specificity (72-98%) in identifying depressive symptoms․ Validation studies confirm its reliability across diverse populations‚ including high-risk and culturally varied groups․ The PDSS also shows strong concurrent validity‚ correlating well with other established measures like the Edinburgh Postnatal Depression Scale (EPDS) and Beck Depression Inventory-II (BDI-II)․ Its clear cutoff scores (e․g․‚ 60 for minor depression‚ 80 for major depression) enhance its clinical utility‚ making it a reliable tool for early detection and intervention in postpartum depression․ Its psychometric strength supports its widespread use in clinical and research settings․
Validation Studies and Cultural Adaptations
Extensive validation studies confirm the PDSS’s reliability across diverse populations․ Research in Turkish‚ Chinese‚ and Spanish-speaking cohorts demonstrates its cross-cultural validity․ Adaptations maintain the original structure while ensuring linguistic accuracy․ Studies show consistent sensitivity (91-94%) and specificity (72-98%) across cultures․ For instance‚ a Turkish adaptation achieved strong internal consistency (Cronbach’s alpha = 0․89)․ Similarly‚ a Spanish version effectively screened postpartum depression among Latin American women․ Cultural adaptations ensure the scale remains effective in identifying at-risk mothers globally‚ supporting its use in varied clinical settings to improve early detection and intervention for postpartum depression worldwide․

Comparison with Other Screening Tools
The PDSS is a 35-item scale‚ unlike the shorter 10-item EPDS․ It provides deeper symptom insight but requires purchase‚ whereas some tools are free‚ balancing detail with accessibility․
PDSS vs; Edinburgh Postnatal Depression Scale (EPDS)
The PDSS and EPDS are both widely used tools for assessing postpartum depression but differ in structure and application․ The PDSS‚ developed by Beck and Gable‚ includes 35 items across seven dimensions‚ offering a comprehensive assessment of symptoms like sleeping disturbances and emotional distress․ In contrast‚ the EPDS‚ created by Cox and Holden‚ is a shorter 10-item tool focusing primarily on emotional symptoms․ While the EPDS is quicker to administer‚ the PDSS provides deeper insight into symptom severity and complexity․ Both tools are validated for postpartum use‚ but the PDSS is specifically designed for this population‚ whereas the EPDS is also used in other postnatal contexts․ The PDSS requires purchase‚ while the EPDS is often free‚ making it more accessible in some settings․ Both tools highlight the importance of early detection but cater to different clinical needs and preferences․
PDSS vs․ Patient Health Questionnaire (PHQ-9)
The PDSS and PHQ-9 are both screening tools for depression but differ in focus and application․ The PDSS is specifically designed for postpartum depression‚ comprising 35 items across seven dimensions‚ such as emotional distress and somatic symptoms․ In contrast‚ the PHQ-9 is a broader‚ 9-item tool assessing general depression symptoms․ While the PDSS provides deeper insights into postpartum-specific issues‚ the PHQ-9 is quicker and more versatile for general populations․ Both tools are validated but cater to different clinical needs․ The PDSS requires purchase‚ whereas the PHQ-9 is freely available‚ making it more accessible for widespread use․ Each tool offers unique advantages‚ with the PDSS excelling in postpartum contexts and the PHQ-9 in broader mental health screening․

Clinical Applications of the PDSS
The PDSS is widely used in clinical settings to identify postpartum depression early‚ enabling timely interventions and improving maternal outcomes․ Its structured format allows for efficient screening during routine postpartum care․
Using PDSS in Clinical Settings
The PDSS is a valuable tool in clinical settings for early detection of postpartum depression․ Its 35-item structure allows healthcare providers to quickly assess symptoms‚ ensuring timely interventions․ In practice‚ the PDSS is often administered during postpartum check-ups‚ taking only 5-10 minutes to complete․ This efficiency makes it ideal for busy clinical environments․ The scale’s self-report format empowers mothers to openly share their emotional experiences‚ fostering trust and accurate assessments․ By identifying high-risk individuals early‚ clinicians can refer them to appropriate resources‚ significantly improving maternal and infant health outcomes․ The PDSS’s specificity and sensitivity ensure reliable results‚ making it a preferred choice for healthcare professionals worldwide․
Integrating PDSS into Routine Postpartum Care
Integrating the PDSS into routine postpartum care enhances early detection of depressive symptoms in mothers․ The scale is typically administered during well-child visits or postpartum check-ups‚ ensuring seamless incorporation into existing workflows․ Its brief‚ 5-10 minute format minimizes disruption to clinical routines while providing critical insights․ By identifying at-risk women early‚ healthcare providers can initiate timely interventions‚ improving maternal and infant health outcomes․ The PDSS is also available in PDF format‚ making it easily accessible for clinicians to use during appointments․ This tool not only aids in early detection but also supports the referral process‚ ensuring women receive the care they need․ Its widespread adoption highlights its practicality and effectiveness in postpartum care settings․

PDSS and Its Availability in PDF Format
The PDSS is available in PDF format‚ making it easily accessible for clinicians to use in various clinical settings․ The PDF version ensures convenience and readability‚ facilitating effective screening․
Accessing the PDSS in PDF
The PDSS is widely available in PDF format‚ enabling easy access for healthcare providers and researchers․ It can be obtained from its publisher‚ Western Psychological Services‚ or through authorized distributors․
The PDF version maintains the scale’s original structure‚ ensuring clarity and readability․ Clinicians can download or print it for use in clinical settings‚ making it a practical tool for routine postpartum care․
Additionally‚ the PDSS PDF is compatible with electronic health records‚ allowing seamless integration into patient documentation systems․ This accessibility ensures widespread use globally‚ aiding in early detection and intervention for postpartum depression․
- Available from Western Psychological Services․
- Designed for easy printing and digital use․
- Compatible with electronic health records․
Using the PDF Version in Practice
The PDSS PDF is a practical tool for clinicians‚ offering a convenient way to assess postpartum depression in clinical settings․ Its structured format allows for quick administration‚ typically taking 5-10 minutes‚ making it ideal for busy healthcare environments․
Healthcare providers can easily print or display the PDF on digital devices‚ ensuring seamless integration into routine postpartum care․ The tool’s clarity and readability facilitate accurate patient responses‚ aiding in early detection of depressive symptoms․
The PDSS PDF is also useful in diverse settings‚ from hospitals to outpatient clinics‚ and can be shared among multidisciplinary teams to ensure comprehensive care․ Its availability in PDF format enhances accessibility‚ making it a valuable resource for improving maternal mental health outcomes․
- Quick and easy to administer in clinical settings․
- Facilitates early detection of postpartum depression․
- Supports comprehensive and coordinated care․
Case Studies and Examples
The PDSS has been successfully applied in high-volume obstetric practices‚ identifying women at risk and improving outcomes through early intervention and cultural adaptations․
Real-World Applications of the PDSS
The PDSS is widely used in clinical settings to identify postpartum depression early‚ ensuring timely interventions and improving maternal mental health outcomes․
Its structured format and ease of administration make it a valuable tool for healthcare providers‚ allowing seamless integration into routine postpartum care visits․
Studies have demonstrated its effectiveness in diverse populations‚ with cultural adaptations enabling its use across different regions and languages‚ thus enhancing its global applicability․
Additionally‚ the PDSS has been utilized in research to assess the prevalence and predictors of postpartum depression‚ contributing to a deeper understanding of this condition․
Success Stories and Outcomes
The PDSS has proven to be an effective tool in identifying postpartum depression early‚ enabling healthcare providers to intervene promptly and improve maternal mental health outcomes․
Studies have shown that women screened with the PDSS and referred for treatment experienced significant reductions in depressive symptoms‚ leading to better overall well-being․
Its implementation in clinical settings has been praised for enhancing the quality of postpartum care‚ ensuring that mothers receive the support they need during a vulnerable period․
Additionally‚ the PDSS has been successfully validated across diverse populations‚ demonstrating its reliability and effectiveness in various cultural and clinical contexts․
By facilitating early detection and appropriate interventions‚ the PDSS has played a crucial role in improving both maternal and child health outcomes worldwide․
The PDSS has proven to be a valuable tool in identifying postpartum depression‚ enabling early intervention and improving maternal mental health outcomes globally․
Future directions include further validation across diverse populations and integration into digital health platforms to enhance accessibility and efficiency in clinical settings․
The Postpartum Depression Screening Scale (PDSS)‚ developed by Beck and Gable in 2000‚ is a 35-item self-report tool designed to assess postpartum depression (PPD) in mothers․ It evaluates seven key dimensions‚ including emotional and psychological symptoms‚ offering a comprehensive yet efficient screening process․ The PDSS is widely recognized for its ability to identify high-risk individuals early‚ enabling timely interventions․ Its structured format and ease of administration (5-10 minutes) make it a valuable resource in clinical settings․ With specific cutoff scores (e․g․‚ 60 for minor depression and 80 for major depression)‚ the PDSS provides clear diagnostic guidance․ Its impact extends beyond individual care‚ contributing to improved maternal mental health outcomes and reducing long-term risks for both mothers and children․
Future Developments and Improvements
Future developments of the Postpartum Depression Screening Scale (PDSS) aim to enhance its accessibility and adaptability․ One potential improvement is making the scale freely available online‚ reducing barriers to its use in resource-limited settings․ Additionally‚ efforts to adapt the PDSS for diverse cultural and linguistic populations could expand its global application․ Integrating digital platforms for easier administration and automated scoring could also streamline its use in clinical workflows․ Further research into its validity across different postpartum periods and populations will strengthen its reliability․ By addressing these areas‚ the PDSS can continue to serve as a critical tool for early detection and intervention in postpartum depression‚ ultimately improving maternal mental health outcomes worldwide․









Leave a Comment